~5 mins
•Jan 2026
Hypothetical Patient Case: 80-Year-Old With Depressive Episodes in Long-Term Care
Interactive Patient Case
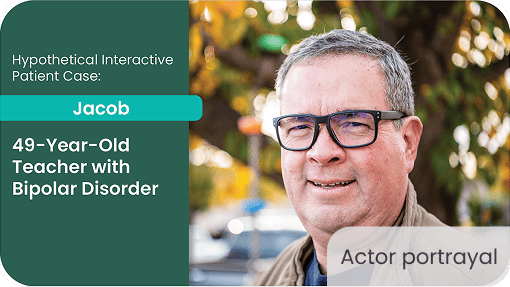
Hypothetical Patient Case: 49-Year-Old Teacher With Bipolar Disorder

~5 mins
•Jan 2026
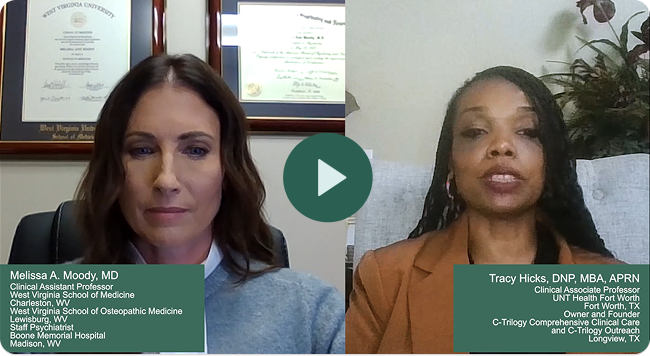
Dr Melissa Moody and Dr Tracy Hicks provide their insight and discuss a case of mild tardive dyskinesia.
Dr Melissa Moody brings a comprehensive approach to patient care with her dual training in psychiatry and internal medicine. Dr Tracy Hicks, a dual-certified APRN in both family practice and psychiatric-mental health, employs a holistic approach to help her patients achieve their goals.

Disclaimer: This is a hypothetical patient case developed for educational purposes by Dr Melissa Moody, MD, and Dr Tracy Hicks, DNP, MBA, APRN, based on characteristics of patients with tardive dyskinesia as seen in clinical practice. The hypothetical case was sponsored and co-developed by Neurocrine Biosciences.
Mild TD is often overlooked and underestimated in clinical practice; even these subtle involuntary movements can significantly affect patients’ quality of life and behavior. This hypothetical case aims to illustrate that impact and to emphasize the importance of recognizing, discussing, and assessing mild TD symptoms. The case includes relevant patient context, thought-provoking questions, and commentary from Dr Melissa Moody and Dr Tracy Hicks.
Dr Moody and Dr Hicks provide their insight and review the case. Dr Moody brings a comprehensive approach to patient care with her dual training in psychiatry and internal medicine. Dr Hicks, a dual-certified APRN in both family practice and psychiatric-mental health, employs a holistic approach to help her patients achieve their goals.

Family members notice a change, but the patient does not
Patient Summary
Patient has been well-controlled on risperidone for ~5 years
Patient has not experienced any new manic episodes within the past few years
No recent medication changes
No history of substance use, including cannabis
Comorbid Conditions
Bipolar disorder
Hypertension
Type 2 diabetes
Obesity
Hyperlipidemia

Current Medications
Risperidone 3 mg daily
Lisinopril 10 mg daily
Metformin XR 1000 mg at bedtime
Atorvastatin 20 mg daily
Patient Summary
Comorbid Conditions
Current Medications
Patient has been well-controlled on risperidone for ~5 years
Patient has not experienced any new manic episodes within the past few years
No recent medication changes
No history of substance use, including cannabis
Bipolar disorder
Hypertension
Type 2 diabetes
Obesity
Hyperlipidemia

Risperidone 3 mg daily
Lisinopril 10 mg daily
Metformin XR 1000 mg at bedtime
Atorvastatin 20 mg daily
XR, extended-release.
Which of the following most closely aligns with how you normally screen a patient like Jacob for TD?
Select all that apply.
AIMS, Abnormal Involuntary Movement Scale; TD, tardive dyskinesia.
Which of the following most closely aligns with how you normally screen a patient like Jacob for TD?
Select all that apply.
Faculty Insights

AIMS, Abnormal Involuntary Movement Scale; TD, tardive dyskinesia.
Jacob is alert with stable vital signs
Examination
Mild, irregular, involuntary lip puckering and tongue movement, most noticeable at rest
No limb, trunk, or respiratory involvement observed
No rigidity, tremor, or bradykinesia
Normal reflexes
AIMS Score: 3 (orofacial area, specifically lip and tongue)
Presentation consistent with mild orofacial TD, secondary to chronic risperidone therapy
AIMS, Abnormal Involuntary Movement Scale; TD, tardive dyskinesia.
Which would you prioritize to ensure Jacob understands his new diagnosis of mild TD?
TD, tardive dyskinesia.
Which would you prioritize to ensure Jacob understands his new diagnosis of mild TD?
Faculty Insights

TD, tardive dyskinesia.
How would you approach treatment for Jacob?
Select all that apply.
TD, tardive dyskinesia; VMAT2, Vesicular Monoamine Transporter 2.
How would you approach treatment for Jacob?
Select all that apply.
TD, tardive dyskinesia; VMAT2, Vesicular Monoamine Transporter 2.
APA, American Psychiatric Association; TD, tardive dyskinesia; VMAT2, Vesicular Monoamine Transporter 2.
Which are the most important considerations you keep in mind when selecting a VMAT2 inhibitor?
Select all that apply.
TD, tardive dyskinesia; VMAT2, Vesicular Monoamine Transporter 2.
Which are the most important considerations you keep in mind when selecting a VMAT2 inhibitor?
Select all that apply.
Faculty Insights
TD, tardive dyskinesia; VMAT2, Vesicular Monoamine Transporter 2.


We hope this discussion has provided valuable insights into the evaluation and management of patients with mild tardive dyskinesia
Disclaimer: This is a hypothetical patient case developed for educational purposes by Dr Melissa Moody, MD, and Dr Tracy Hicks, DNP, MBA, APRN, based on characteristics of patients with tardive dyskinesia as seen in clinical practice. The hypothetical case was sponsored and co-developed by Neurocrine Biosciences.
By continuing to use this site, you agree to our use of cookies as described in our Cookie Policy.